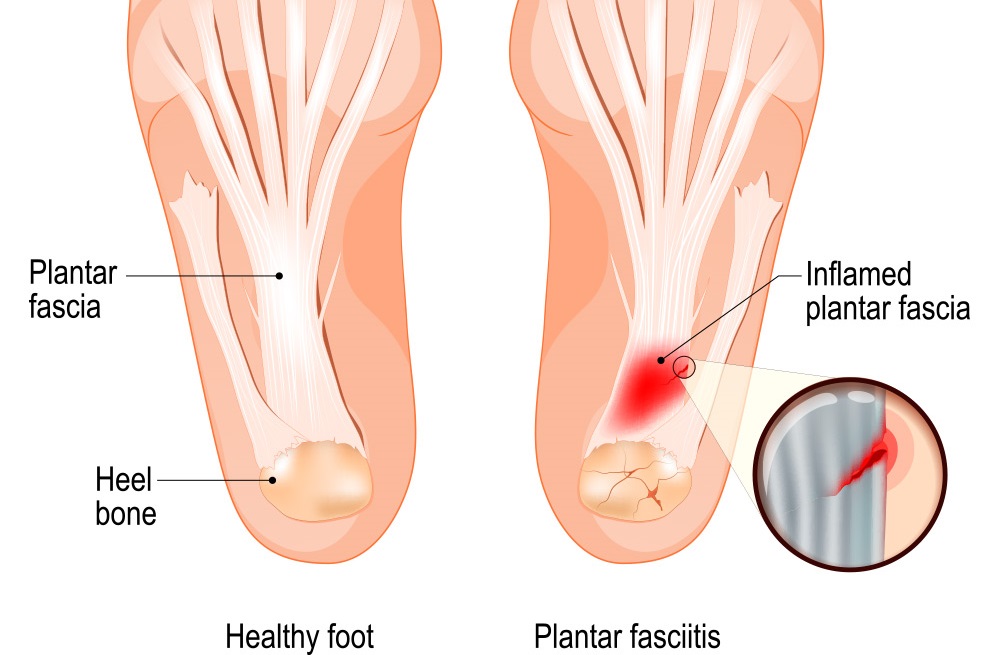
Plantar fasciitis is a condition which affects the sole of your foot. The condition has many names in which it may be referred to; these include Plantar fasciosis, plantar heel pain, and plantar fascial fibramatosis.
The plantar fascia is made up of fibrous connective tissue which originates on the medial calcaneal tubercle (heel bone), and splits into five bands as it attaches to all 5 metatarsal heads (toes). Pain can be felt where the fascia joins the heel bone (insertional) or in the central portion (non insertional). The plantar fascia joins the paratenon of the Achilles tendon, foot muscles and the skin and subcutaneous tissue.

The foot absorbs up to 110% of body weight while walking and 250% while running. The plantar fascia deforms most during barefoot walking vs. shoe walking. During walking or running the tibia (shin bone) loads the foot and creates tension through the plantar fascia, this called the windlass mechanism. The tension created in the plantar fascia adds critical stability to the loaded foot and minimises muscle activity.
Prognosis
Evidence states that episodes of plantar heel pain last longer than 6 months and it affects 10-15% of the population. However, approximately 90% of cases are treated successfully with conservative care.
Causative Factors
This condition is most common in the middle aged, women, and the athletic population. However it can occur outside these parameters. It makes up 8-10% of all running related injuries.
Other risk factors which contribute to plantar heel pain including but not limited too:
- Loss of ankle range of motion (dorsi flexion)
- Flat feet or high arches
- Excessive foot pronation dynamically
- Impact/weight bearing activities such as prolonged standing, running, etc
- Improper shoe fit
- Elevated BMI > kg/m2
- Metabolic conditions such as Diabetes Mellitus
Symptoms
- Heel pain with first steps in the morning or after long periods of non-weight bearing
- Tenderness to the anterior medial (inside) heel
- Limited dorsi flexion (ankle ROM) and tight Achilles tendon
- A limp may be present or may have a preference to toe walking
- Pain is usually worse when barefoot on hard surfaces and with stair climbing
- Many patients may have had a sudden increase in their activity level prior to the onset of symptoms
Diagnosis
The condition can be diagnosed clinically through a comprehensive subjective and objective assessment by your physiotherapist at Get Active Physiotherapy. In rare cases further investigation such as radiographs, diagnostic ultrasound or MRI may be required.
Physiotherapy Management
– Stretching- gastroc/soleus (calf), plantar fascia,
– Soft tissue releases/massage and joint mobilisations
– Orthotics
– Night splints
– Specific Strength training
Here at Get Active we can provide you with the best individualised treatment options to optimise a speedy recovery.
If you have any questions or would like to book in to see one of our physiotherapists, please do not hesitate to contact Get Active Physiotherapy on 1300 8 9 10 11 or email us at admin@getactivephysio.com.au